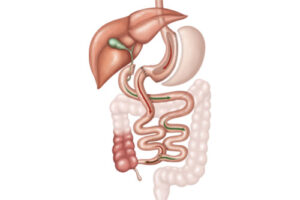
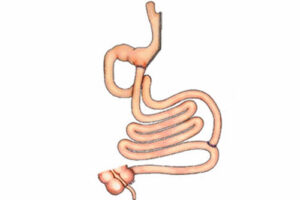
IIP: ileal interposition surgery with open or closed surgical methods (iip: ileal interposition surgery (closure of the duodenum made from multiple holes, cutting 170 cm from the last part of the ileum and joining these opened ends and joining the lower part of the duodenum with the jegenum of the remaining ileum). The surgical method that aims to lose weight by eating less and meanwhile mouthing the upper part of the small intestine called the ileum to the upper part of the small intestine called jejenum and mouthing the upper part of the ileum to the duodenum, thus reducing the absorption of food into the small intestine partially and early stimulation of insulin secretion, the surgical method that aims to treat diabetes, diet and sports. It can help to lose weight and control diabetes.
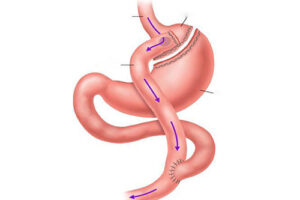
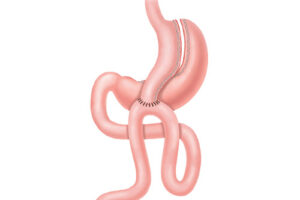
The surgery to be performed is schematically below. In these operations, by using two different mechanisms (OPEN AND CLOSED METHOD), effective weight loss / diabetes control is achieved. These operations can be performed by open surgical methods by cutting the anterior abdominal wall, as well as by laparoscopic (closed) method by inflating with intraabdominal carbon dioxide gas in the presence of cameras and surgical instruments inserted through 5-8 holes with a diameter of only 0.5-1.5 cm. Openings in the abdominal skin will be closed aesthetically.
After this operation, there will be no change in the main lines of obesity and diabetes treatment (such as special nutrition plans, continuing diet and exercising, staying under the supervision of a dietician for a long time). Nutrition with liquid foods is required for at least 3 weeks after the operation. Later, the weight loss procedure will continue with the support of special diet and intervals to control body functions. More detailed information on the subject has been explained to you by me.
This form contains your detailed information about the surgery and the next period and your consent on this issue
Pictures Used in Information (1st Picture is the operation preparation, 2nd is after)
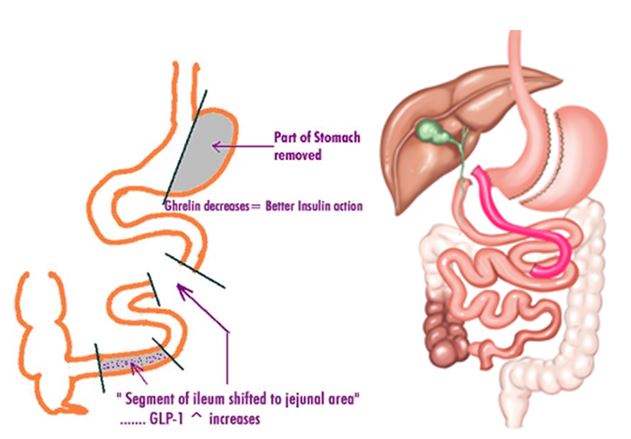
This surgery is the operation of closing the duodenum from 1 continent with multiple holes or open surgical intervention, cutting the ileum 170 cm from the last part, separating the ends in a way that will not disturb the nutrition and joining the ends of this small intestine (ileum) and joining the upper part of the separated small intestine (ileum) with the lower part of the duodenum.
✓ GLP-1 is secreted early in the passage of food, as the lower part called ileum is added to the stomach outlet to meet the food first. This stimulates insulin release from the pancreas
✓ In addition, the mechanism creates a more effective insulin effect by eliminating the insulin drain.
Possible Results After Surgical Treatment: We Expect:
With Sleeve gastrectomy, which is a part of IIP, the volume of your stomach, which is reduced to a tube or banana, decreases. Your food portions are smaller. For example, while eating a plate of soup, 5-6 pieces of meatballs, rice or pasta and salad before the surgery and feeling that you are full; After the operation, you will be saturated with 4 spoons of soup and one meatball.
Hunger hormone secreted from the removed part of your stomach decreases by 70-80% after sleeve gastrectomy surgery. The name of this hormone is ghrelin. You will feel less hungry between meals thanks to the reduction of the hunger hormone. Your feeling of fullness lasts longer.
Because your stomach is tubed with sleeve gastrectomy, your stomach empties faster. The rapid passage of the foods eaten from the stomach to the small intestine can also increase your bowel movements. Although sleeve gastrectomy does not make any changes in your intestines, some excess calories of foods are discarded without being absorbed, partially due to increased bowel movements.
Most of the patients state that they do not feel their old cravings for different foods they used to like. In fact, they do not want to eat some foods because their taste deteriorates. Frequently mentioned among such foods are coffee, cola, some pastries and cookies.
The part of the stomach near the exit is called Antrum. At the end of sleevegastrectomy (gastric tubing), the pressure of the antrum, which is the exit part of the stomach, increases. This increase in pressure causes the antrum to stretch and suppress the feeling of hunger.
Since sleeve gastrectomy does not leave a foreign body inside, problems related to this are not encountered.
IIP will change the anatomy of the digestive system.
In Sleeve Gastrectomy, the part of the stomach that stretches the most and enlarges the stomach volume is removed. The remaining stomach part does not stretch too much. Therefore, it prevents overeating.
Making the stomach into a tube increases the resistance of the stomach to food. It does not allow the passage of extremely large volumes of food. The bites of the food you eat become smaller.
Tubing of the stomach allows the food entering the stomach to be rapidly evacuated from the stomach. Foods that cannot stay in the stomach for a long time leave the stomach before they find the time to enlarge the stomach volume.
The passage of food to the small intestine is accelerated by gastric tubing. This rapid transition stimulates movement in the small intestine. Although Sleeve Gastrectomy does not make any changes in the small intestines, it also prevents excessive absorption of calories taken with food in this way.
As the duodenum outlet from the lower part of the pylorus and the lower part of the small intestine are made up, food absorption decreases. However, since the pylorus is preserved, dumpings syndrome and diastolic are either rare or absent.
Changes in the small intestine can cause gas pain from time to time.
Since it increases in insulin secretion, the effect of insulin increases, the need decreases and the insulin production power of the pancreas increases. This will be an advantage for controlling diabetes.
✓ Especially in patients who are immobile for a long time, those who have obesity problems and those who use drugs that increase the chance of blood clotting, with pain and swelling, clot formation in the legs (deep ventrombosis or DVT). In very rare cases, this clot can break off from its location and travel to the lungs.
Heart attack or heart failure due to heart strain
✓ Problems with the central nervous system and stroke.
✓ Death that may result from the procedure.
✓ Increased risk of wound infection, lung infection, heart and lung complications, coagulation in obese (overweight) patients.
✓ Increased risk of wound infection, lung infection, heart and lung complications, coagulation in smoking patients.
✓ Attacks and problems that may occur in patients with previously known systemic diseases such as diabetes and hypertension.
✓ The development of problems due to the pushing of the heart upwards during the operation in patients with lung failure, heart failure and heart rhythm disorder due to the increase in intraabdominal pressure during laparoscopic operations.
✓ Other information
✓ Death after major surgery
✓ Inflammatory accumulation in the abdomen, abscess
✓ Allergic reactions
✓ Anesthesia complications
✓ Bleeding
✓ Deep vent thrombosis and pulmonary embolism
✓ Intestinal obstruction, Herniation and herniation between internal organs
✓ Return to open surgery
✓ Depression
✓ Difficulty swallowing
✓ Hair loss
✓ Infection
✓ Perforation intestinal leak
✓ Spleen injury
✓ Urinary tract infection
✓ Postoperative inflammation may develop in the abdomen or in the wound. These may in some cases require repeat surgery or minor surgical interventions.
✓ During the surgery, organ injuries such as stomach, pancreas, duodenum, small and large intestine, liver, gall bladder and tracts, spleen, kidney, bladder and large vessels may occur, and these injuries may require additional interventions as these injuries are life-threatening.
✓ If the conditions are not suitable for laparoscopic (closed) operations and if there is a danger to the patient's health, open surgery will be started. This probability is around 1-5%.
✓ Leaks and stitches may occur on the cut and stitched stomach and intestinal walls and may progress with reoperation, long-term hospitalization and even life-threatening. This situation may require additional surgeries or interventions (such as stents).
✓ All necessary measures will be taken to prevent these problems from occurring, but in the presence of such a situation, many surgical interventions may be required later and in the worst case the patient may be lost.
✓ In open surgery, herniation may develop in the early or late period as a result of long-term discharge at the operation site and the melting of the fat tissues under the skin and the partial or complete opening of the wound.
✓ After laparoscopic (closed) surgeries, hernias may rarely occur at the insertion points of the instruments and other surgical interventions may be required for their repair.
✓ It has been reported that there is an increased risk of stone formation in the gallbladder in the long term.
✓ Leakage from Stomach Suture Line: Part of the stomach is removed during sleevegastrectomy surgery. A suture line remains in the stomach whose volume has been reduced. In some cases, there may be small leaks from this suture line. This risk is less than 1%. Many of the leaks that occur are healing without being noticed. In some cases, small abscesses may develop due to these leaks. In these cases, the problem is solved by evacuation of the abscess from the outside and appropriate antibiotic treatment. In rare cases, appropriate treatment may be required with repeat surgery. The causes of these leaks that may occur from the stomach may be related to both the surgical technique and the problems of the patient. Today, various methods have been developed and applied surgically for the safety of the suture line. These methods are used differently by each surgeon. The reasons belonging to the patient are mostly due to the burden of obesity. Obesity itself can cause the immune system to weaken. This may cause a longer and more difficult recovery of the surgically created trauma.
✓ In duodeno-ilealanstomosis, there may be leakage, anastomotic separation, biliary fistula or stenosis. This may prolong the length of hospital stay, cause new surgeries or interventions, and even result in complications such as sepsis despite treatment. The leakage rate is around 1%
✓ In the duodenum stump, leakage, opening in the suture lines and biliary fistula may occur. This complication rate is roughly 1-2%. This complication may prolong the length of hospital stay, cause new surgeries or interventions, and even result in death from complications such as sepsis despite treatment.
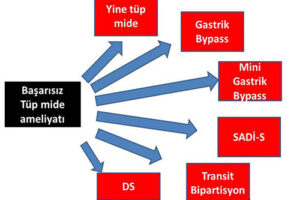
✓ The complications that may occur in the stump and anastomosis can be transformed into other obesity and diabetes surgeries during the operations performed on the body. (Like gastric bypass)
✓ Risk of leak in small bowel anastomoses.
Prof. Dr. Haluk Recai ÜNALP was born in 1963 in Merzifon. In 1987 he graduated from Ankara GATA Medical Faculty.
Until 1987-1990, Keşan served as the Chief Physician and Health Branch Manager of the 4th Infantry Division, and in 2015 he received the title of Professor.
Until 1987-1990, worked in Keşan as the Chief Physician and Health Branch Manager, and in 2015 he received the title of Professor.
İstanbul İrtibat: +90 (544) 422 32 04
İzmir İrtibat: +90 (544) 422 32 03
Tel: +90 (232) 422 32 02
Eposta: info@halukunalp.com
Lokasyon: Haritaya Gözat